Volume 22, Issue 6 (February & March 2020)
J Arak Uni Med Sci 2020, 22(6): 218-229 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ghane M, Adham F. Frequency of TEM and PER Beta-Lactamase Genes in Urinary Isolates of Escherichia Coli Producing Extended-Spectrum Beta-Lactamases. J Arak Uni Med Sci 2020; 22 (6) :218-229
URL: http://jams.arakmu.ac.ir/article-1-6064-en.html
URL: http://jams.arakmu.ac.ir/article-1-6064-en.html
1- Department of Biology, Islamshahr Branch, Islamic Azad University, Islamshahr, Iran. , ghane@iiau.ac.ir
2- Department of Biology, Islamshahr Branch, Islamic Azad University, Islamshahr, Iran.
2- Department of Biology, Islamshahr Branch, Islamic Azad University, Islamshahr, Iran.
Full-Text [PDF 2530 kb]
(1024 Downloads)
| Abstract (HTML) (2384 Views)
Full-Text: (1718 Views)
Extended Abstract
Introduction
Urinary tract infection (UTI) is one of the most important infectious diseases in society and also in hospitals and Escherichia coli is one of the most important causes of UTI. Among antibiotics, β-lactam antibiotics are the most widely used chemotherapeutic drugs due to its non-toxicity [4]. Unfortunately due to the overuse of antibiotics, today we are seeing an increase in strains resistant to these antibiotics. Production of β-lactamase enzymes is one of the most important mechanisms of resistance to this class of antibiotics. Extended-spectrum β-lactamases (ESBLs) are enzymes that cause resistance to broad-spectrum cephalosporins, and as these enzymes are encoded by the plasmid, bacterial resistance is rapidly spread because of these enzymes. These plasmids often carry genes resistant to other antibiotics as well such as aminoglycosides, fluoroquinolones, tetracycline, chloramphenicol and trimethoprim-sulfamethoxazole [5]. TEM-type ESBLs are one of the most important plasmid β-lactamases belonged to enterobacteriaceae family and one of the important causes of multidrug resistance in nosocomial infections [6]. PER enzymes are another type of ESBLs identified first in Pseudomonas aeruginosa but have also been identified in other organisms, especially in Acinetobacter isolates [7]. Treatment of UTI often begins experimentally based on the reports of antibiotic resistance patterns of urinary pathogens. Continuous presentation of antibiotic resistance patterns in each region can prevent the spread of resistant strains in addition to treating UTIs. In this regard, the purpose of this study was to determine the prevalence of Escherichia coli producing ESBLs isolated from the urine of patients with UTI, to determine their susceptibility to common antibiotics used in UTI treatment, and to evaluate the frequency of blaTEM and blaPER β-lactamase genes.
Materials and Methods
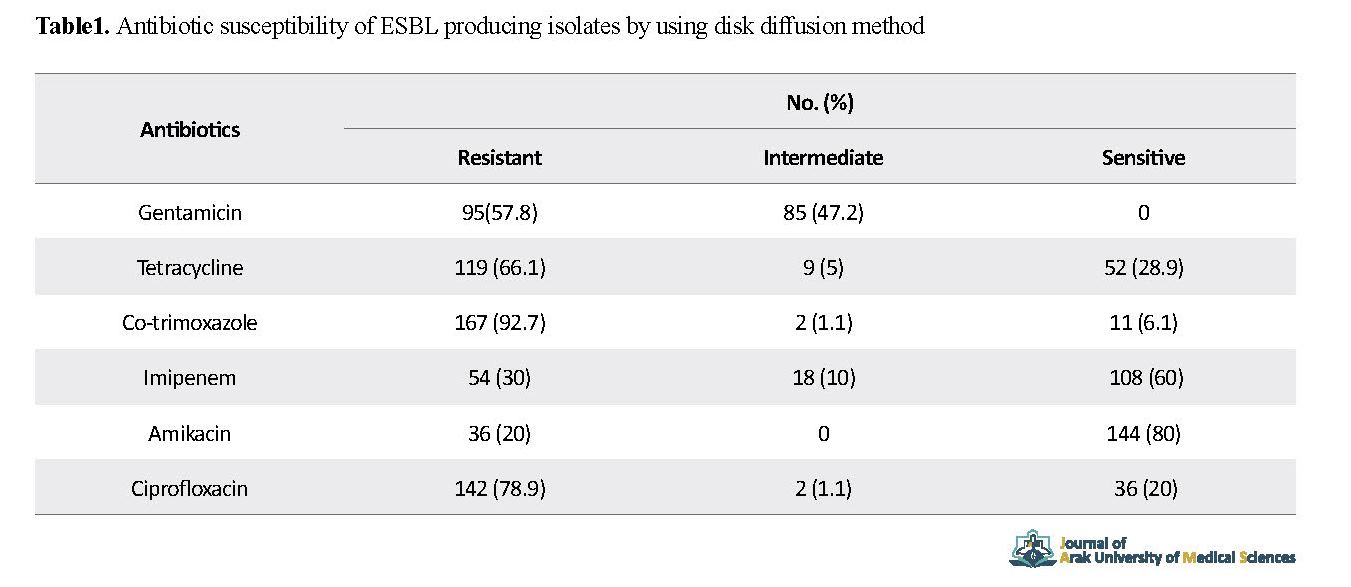
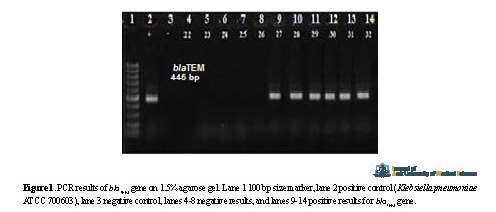
This study was conducted over a period of 13 months (from January 2016 to February 2017) on 972 samples with a suspected UTI extracted from among outpatients referred to hospitals of Imam Khomeini, Qaem, and Shahid Rajaei and laboratories in Karaj, Iran. Urine samples were inoculated on blood agar and eosin methylene blue agar (Merck, Germany). After incubation at 37 ° C for 24 h, plates with remarkable growth (105 cfu /ml) were selected for subsequent experiments. Bacteria were identified based on their morphological and biochemical properties [8]. Screening of Escherichia coli strains producing ESBLs were performed using disk diffusion method and two pairs of disc including cefotaxime (30 µg) and cefotaxime/clavulanic acid (30/10 µg) disks as well as ceftazidime (30 µg) and ceftazidime/Clavulanic acid (30/10 µg) disks (Rosco Company, Denmark) and in accordance with the recommendations of the Clinical and Laboratory Standard Institute (CLSI). Antibiotic susceptibility assessment of strains producing ESBLs was carried out using gentamicin (10 µg), tetracycline (30 µg), trimethoprim sulfamethoxazole (25 µg), imipenem (10 µg), amikacin (30 µg) and ciprofloxacin (5 µg) antibiotics (Rosco, Denmark). For molecular identification of blaTEM and blaPER genes, after genomic DNA extraction, polymerase chain reaction (PCR) experiments were performed using specific primers [10, 11]. Statistical analysis were conducted in SPSS v. 20 software using chi-square test considering a significance level of p<0.05.
Results
Out of 972 suspected samples, 780 infectious samples were diagnosed of which 500 Escherichia coli isolates were isolated. Mean age of patients was 45±16 years. Of these, 169 (33.8%) were male and 331 (66.2%) were female. Out of 500 Escherichia coli isolates, 180 (36%) were positive for β-lactamase production. The number of ESBL strains was higher in females (73.33%; n=132) than in males (26.67%, n=48) (p = 0.007). The results of antibiotic susceptibility testing showed that the strains producing ESBLs were highly resistant to co-trimoxazole and ciprofloxacin (Table 2). The results of TEM β-lactamase gene analysis using specific primers (Figure 1) showed that blaTEM gene was present in 85 (44.72%) of isolates whereas blaRER gene were not present in any of the isolates.
Introduction
Urinary tract infection (UTI) is one of the most important infectious diseases in society and also in hospitals and Escherichia coli is one of the most important causes of UTI. Among antibiotics, β-lactam antibiotics are the most widely used chemotherapeutic drugs due to its non-toxicity [4]. Unfortunately due to the overuse of antibiotics, today we are seeing an increase in strains resistant to these antibiotics. Production of β-lactamase enzymes is one of the most important mechanisms of resistance to this class of antibiotics. Extended-spectrum β-lactamases (ESBLs) are enzymes that cause resistance to broad-spectrum cephalosporins, and as these enzymes are encoded by the plasmid, bacterial resistance is rapidly spread because of these enzymes. These plasmids often carry genes resistant to other antibiotics as well such as aminoglycosides, fluoroquinolones, tetracycline, chloramphenicol and trimethoprim-sulfamethoxazole [5]. TEM-type ESBLs are one of the most important plasmid β-lactamases belonged to enterobacteriaceae family and one of the important causes of multidrug resistance in nosocomial infections [6]. PER enzymes are another type of ESBLs identified first in Pseudomonas aeruginosa but have also been identified in other organisms, especially in Acinetobacter isolates [7]. Treatment of UTI often begins experimentally based on the reports of antibiotic resistance patterns of urinary pathogens. Continuous presentation of antibiotic resistance patterns in each region can prevent the spread of resistant strains in addition to treating UTIs. In this regard, the purpose of this study was to determine the prevalence of Escherichia coli producing ESBLs isolated from the urine of patients with UTI, to determine their susceptibility to common antibiotics used in UTI treatment, and to evaluate the frequency of blaTEM and blaPER β-lactamase genes.
Materials and Methods
This study was conducted over a period of 13 months (from January 2016 to February 2017) on 972 samples with a suspected UTI extracted from among outpatients referred to hospitals of Imam Khomeini, Qaem, and Shahid Rajaei and laboratories in Karaj, Iran. Urine samples were inoculated on blood agar and eosin methylene blue agar (Merck, Germany). After incubation at 37 ° C for 24 h, plates with remarkable growth (105 cfu /ml) were selected for subsequent experiments. Bacteria were identified based on their morphological and biochemical properties [8]. Screening of Escherichia coli strains producing ESBLs were performed using disk diffusion method and two pairs of disc including cefotaxime (30 µg) and cefotaxime/clavulanic acid (30/10 µg) disks as well as ceftazidime (30 µg) and ceftazidime/Clavulanic acid (30/10 µg) disks (Rosco Company, Denmark) and in accordance with the recommendations of the Clinical and Laboratory Standard Institute (CLSI). Antibiotic susceptibility assessment of strains producing ESBLs was carried out using gentamicin (10 µg), tetracycline (30 µg), trimethoprim sulfamethoxazole (25 µg), imipenem (10 µg), amikacin (30 µg) and ciprofloxacin (5 µg) antibiotics (Rosco, Denmark). For molecular identification of blaTEM and blaPER genes, after genomic DNA extraction, polymerase chain reaction (PCR) experiments were performed using specific primers [10, 11]. Statistical analysis were conducted in SPSS v. 20 software using chi-square test considering a significance level of p<0.05.
Results
Out of 972 suspected samples, 780 infectious samples were diagnosed of which 500 Escherichia coli isolates were isolated. Mean age of patients was 45±16 years. Of these, 169 (33.8%) were male and 331 (66.2%) were female. Out of 500 Escherichia coli isolates, 180 (36%) were positive for β-lactamase production. The number of ESBL strains was higher in females (73.33%; n=132) than in males (26.67%, n=48) (p = 0.007). The results of antibiotic susceptibility testing showed that the strains producing ESBLs were highly resistant to co-trimoxazole and ciprofloxacin (Table 2). The results of TEM β-lactamase gene analysis using specific primers (Figure 1) showed that blaTEM gene was present in 85 (44.72%) of isolates whereas blaRER gene were not present in any of the isolates.
Discussion
Over the past decades, gram-negative bacilli producing ESBLs have emerged as important pathogens in nosocomial and community-acquired infections worldwide. Knowing the antibiotic resistance of these strains and their prevalence in each region can help control these microorganisms and prevent them from spreading. The study was performed on 972 urine samples. Of the tested samples, 780 were diagnosed as infectious, and Escherichia coli was the most common bacteria (64.1%) extracted from among patients with UTI. Similar results have been reported in other studies conducted in Iran and other countries [13, 14].
Over the past decades, gram-negative bacilli producing ESBLs have emerged as important pathogens in nosocomial and community-acquired infections worldwide. Knowing the antibiotic resistance of these strains and their prevalence in each region can help control these microorganisms and prevent them from spreading. The study was performed on 972 urine samples. Of the tested samples, 780 were diagnosed as infectious, and Escherichia coli was the most common bacteria (64.1%) extracted from among patients with UTI. Similar results have been reported in other studies conducted in Iran and other countries [13, 14].
The results of this study showed that the prevalence of UTI in women was significantly higher than in men. These results are consistent with other studies in Iran and other countries [14, 16]. Women are more susceptible to UTI due to colonization of the gram-negative bacteria due to proximity of the anus and urinary tract. The majority of ESBL-producing strains were also found among women (P = 0.007).
The prevalence of ESBL-positive strains in our study was 36%. Its prevalence rate has been reported different in different countries and even in different hospitals. This is due to differences in treatment regimen applied in different regions. Overuse of antibiotics, especially cephalosporins, is one of the most important causes of the high prevalence of ESBL-producing strains.
In this study, ESBL-producing strains showed high resistance to ciprofloxacin. Studies in Iran have shown that ciprofloxacin is prescribed more than other antibiotics to treat UTI. This may contribute to an increase in the prevalence of antibiotic-resistant isolates. The results of this study indicate that this drug as an experimental antibacterial drug, cannot have the appropriate effect. High resistance to aminoglycosides, carbapenems and cotrimoxazole was observed in our study, which was higher compared to other studies in Iran and other countries. ESBL production is usually associated with resistance to several antibiotics. Since ESBL genes are encoded by plasmids, they usually carry genes resistant to other antibiotics as well. One worrying outcome of this study was the high resistance to carbapenems. Although most studies have indicated imipenem as a suitable drug to treat infections caused by ESBL-producing strains, the isolates in our study showed high resistance to imipenem. In this study, 47.2% of isolates had TEM gene. Similarly, in studies conducted in India, 47.93% of ESBL-producing isolates had TEM gene, while prevalence of TEM genes in Thailand was 31.93%. Antibiotics used in a hospital or region can affect the distribution of resistance genotypes.
Escherichia coli was isolated as the most common cause of UTI. The majority of ESBL-producing strains were resistant to most of the antibiotics used to treat UTI. A high percentage of these strains were resistant to imipenem and hence, imipenem has no effect on treatment. The findings of this tsudy raise concerns about the release of ESBL-producing Escherichia coli strains and emphasize their detection in medical diagnostic laboratories and careful monitoring of their resistance patterns.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Research Ethics Committee of Islamic Azad University of Tehran Medical Branch (Code: IR.IAU.TMU.REC.1396.274).
Funding
This study was derived from an MSc. thesis funded by the Islamic Azad University, Islamshahr branch, Islamshahr, Iran.
Authors' contributions
Conceptualization, methodology, validation, supervision, data analysis, initial draft preparation, editing and review: Maryam Ghane; Investigation, resources, experiments and analysis: Fariba Adham.
Conflicts of interest
The authors declare no conflict of interest.
Acknowledgements
This study was extracted from the master thesis of Fariba Adham approved by the Islamic Azad University of Eslamshahr Branch.
The prevalence of ESBL-positive strains in our study was 36%. Its prevalence rate has been reported different in different countries and even in different hospitals. This is due to differences in treatment regimen applied in different regions. Overuse of antibiotics, especially cephalosporins, is one of the most important causes of the high prevalence of ESBL-producing strains.
In this study, ESBL-producing strains showed high resistance to ciprofloxacin. Studies in Iran have shown that ciprofloxacin is prescribed more than other antibiotics to treat UTI. This may contribute to an increase in the prevalence of antibiotic-resistant isolates. The results of this study indicate that this drug as an experimental antibacterial drug, cannot have the appropriate effect. High resistance to aminoglycosides, carbapenems and cotrimoxazole was observed in our study, which was higher compared to other studies in Iran and other countries. ESBL production is usually associated with resistance to several antibiotics. Since ESBL genes are encoded by plasmids, they usually carry genes resistant to other antibiotics as well. One worrying outcome of this study was the high resistance to carbapenems. Although most studies have indicated imipenem as a suitable drug to treat infections caused by ESBL-producing strains, the isolates in our study showed high resistance to imipenem. In this study, 47.2% of isolates had TEM gene. Similarly, in studies conducted in India, 47.93% of ESBL-producing isolates had TEM gene, while prevalence of TEM genes in Thailand was 31.93%. Antibiotics used in a hospital or region can affect the distribution of resistance genotypes.
Escherichia coli was isolated as the most common cause of UTI. The majority of ESBL-producing strains were resistant to most of the antibiotics used to treat UTI. A high percentage of these strains were resistant to imipenem and hence, imipenem has no effect on treatment. The findings of this tsudy raise concerns about the release of ESBL-producing Escherichia coli strains and emphasize their detection in medical diagnostic laboratories and careful monitoring of their resistance patterns.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Research Ethics Committee of Islamic Azad University of Tehran Medical Branch (Code: IR.IAU.TMU.REC.1396.274).
Funding
This study was derived from an MSc. thesis funded by the Islamic Azad University, Islamshahr branch, Islamshahr, Iran.
Authors' contributions
Conceptualization, methodology, validation, supervision, data analysis, initial draft preparation, editing and review: Maryam Ghane; Investigation, resources, experiments and analysis: Fariba Adham.
Conflicts of interest
The authors declare no conflict of interest.
Acknowledgements
This study was extracted from the master thesis of Fariba Adham approved by the Islamic Azad University of Eslamshahr Branch.
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |