BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://jams.arakmu.ac.ir/article-1-6203-en.html
2- Department of Periodontology, Faculty of Dentistry, Arak University of Medical Sciences, Arak, Iran. , mbayani@gmail.com
Introduction
Periodontitis is one of the most common chronic inflammatory diseases that can affect anyone of any age. The cause of periodontitis is the presence of opportunistic bacteria that are naturally present in the mouth [1]. Periodontitis is a multifactorial disease that is affected by various factors [8]. Risk assessment for chronic diseases is very important because it is common in a small group of people who are at higher risk [9]. Various factors have been identified that cause periodontitis, including weakened immune systems, smoking [10], alcohol abuse, and personal oral health [12]. The aim of this study was to evaluate some of the risk factors for periodontitis including smoking, alcohol use, toothbrushing and Socioeconomic Status (SES).
Materials and Methods
This case-control study was conducted on 240 students of Arak University of Medical Sciences (120 periodontitis patients and 120 healthy peers). Two questionnaires were used to collect information; a demographic and risk factors form, and a questionnaire prepared by Garmaroodi et al. to assess the SES of participants. To diagnose periodontitis, the identification of the areas with dental plaque accumulation and clinical examination were used. The criteria for periodontitis included the observation of teeth with any periodontal disease, the observation of bone loss on radiography images, and the probing depth ≥4 mm. Multilevel logistic regression was used to investigate the relationship between periodontitis and other variables. Data were analyzed in Stata 11 software.
Results
Demographic information and risk factors related to study participants are shown in Table 1,
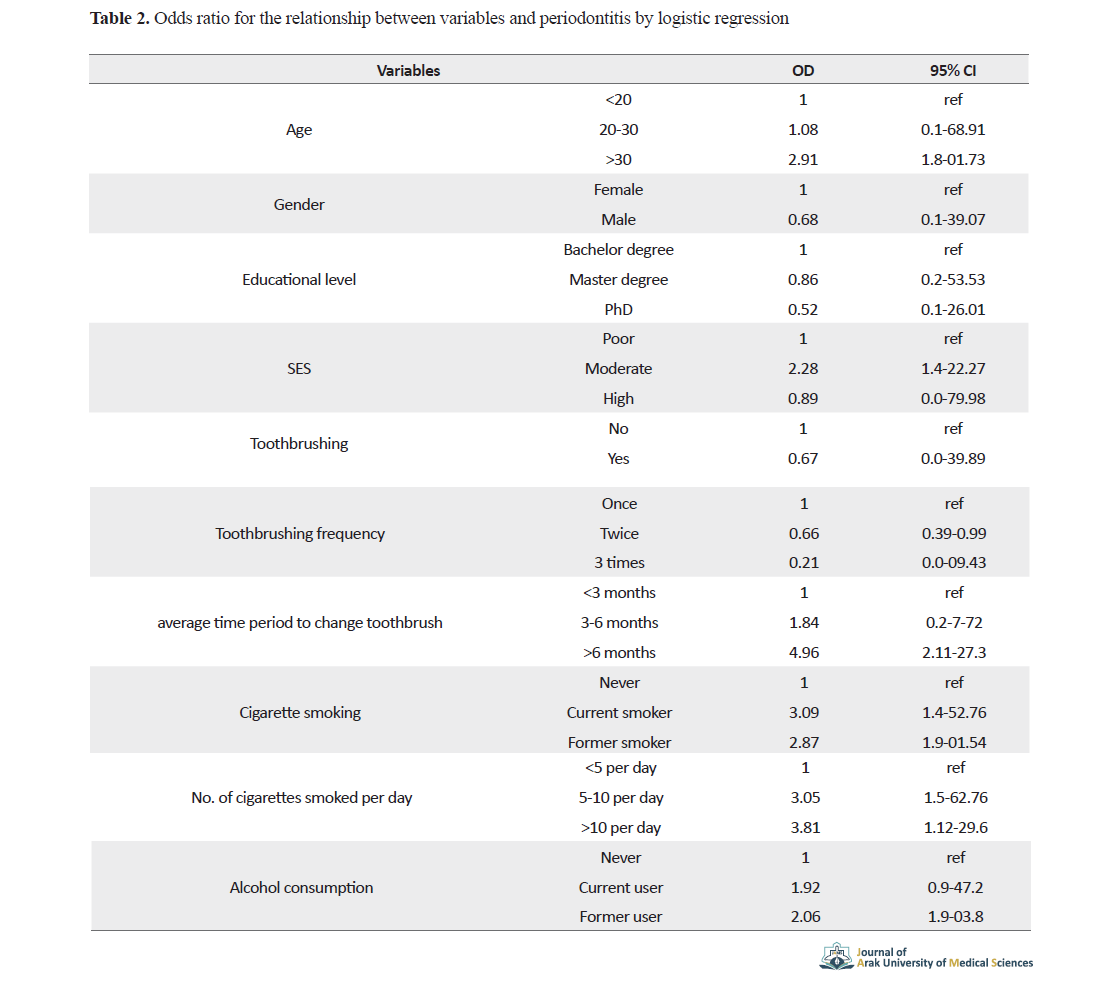
and the relationship between periodontitis and study variables using multilevel logistic regression are presented in Table 2.
According to Odds Ratio (OR) values, the relationship of Periodontitis with age (>30 years vs. <20 years), SES (poor vs. moderate and high), toothbrushing, the average time period to change toothbrush (<3 months vs. >6 months), and cigarette smoking was significant. The dose-response relationship for cigarette smoking and periodontitis was also significant, where the chance of developing periodontitis was OR= 3.05 among patients who smoked 5-10 cigarettes per day, and OR= 3.81 among those who smoked more than 10 cigarettes per day, compared to those who smoked less than 5 cigarettes per day.
Discussion
In this study, there was a significant relationship between prevalence of periodontitis and smoking, toothbrushing, toothbrush replacement, and SES. There was also a dose-response relationship for cigarette smoking. As the number of smoked cigarettes increased, the risk of periodontitis also increased. Being a former or current smoker also affects periodontitis. In different studies, similar results have been reported for smoking, although the effects of previous and current smoking have not been studied [20-23]. People who smoke more than 10 cigarettes a day are more likely to develop periodontitis [27]. Periodontitis prevalence was highest in current smokers, low in former smokers, and lowest in those who had never smoked [29]. People with high SES had higher periodontal health than people with poor SES [16]. Alcohol consumption increases the risk of periodontitis [31]. On average, people consuming alcohol less than once a week are just as likely to develop periodontitis as those who do not drink alcohol [32]. Alcohol consumption also has a significant effect on clinical attachment level [36].
Conclusion
Given the importance of periodontitis, its various complications and high costs, and given the role of its risk factors, it is necessary to plan to reduce cigarette smoking and alcohol consumption and increase oral health and brushing, especially in young people.
Ethical Considerations
Compliance with ethical guidelines
This study obtained its ethical approval from the Research Ethics Committee of Arak University of Medical Sciences (Code: 1397.145).
Funding
The present paper was extracted from the PhD thesis of the first author Department of Periodontology, Faculty of Dentistry, Arak University of Medical Sciences.
Authors' contributions
All authors met the writing standards based on the recommendations of the International Committee of Medical Journal Editors (ICMJE).
Conflicts of interest
The authors declared no conflict of interest.
The authors would like to thank the Deputy for Research of Arak University of Medical Sciences for their financial support.
References
1.Shi M, Wei Y, Hu W, Nie Y, Wu X, Lu R. The subgingival microbiome of periodontal pockets with different probing depths in chronic and aggressive periodontitis: A pilot study. Front Cell Infect Microbiol. 2018; 8:124. [DOI:10.3389/fcimb.2018.00124] [PMID] [PMCID]
2.Haworth S, Shungin D, Kwak SY, Kim HY, West NX, Thomas SJ, et al. Tooth loss is a complex measure of oral disease: Determinants and methodological considerations. Community Dent Oral Epidemiol. 2018; 46(6):555-62. [DOI:10.1111/cdoe.12391] [PMID] [PMCID]
3.Ding Y, Ren J, Yu H, Yu W, Zhou Y. Porphyromonas gingivalis, a periodontitis causing bacterium, induces memory impairment and age-dependent neuroinflammation in mice. Immun Ageing. 2018; 15(1):6. [DOI:10.1186/s12979-017-0110-7] [PMID] [PMCID]
4.Leys EJ, Lyons SR, Moeschberger ML, Rumpf RW, Griffen AL. Association of bacteroides forsythus and a novel bacteroides phylotype with periodontitis. J Clin Microbiol. 2002; 40(3):821-5. [DOI:10.1128/JCM.40.3.821-825.2002] [PMID] [PMCID]
5.Luan X, Zhou X, Naqvi A, Francis M, Foyle D, Nares S, et al. MicroRNAs and immunity in periodontal health and disease. Int J Oral Sci. 2018; 10(3):1-14. [DOI:10.1038/s41368-018-0025-y] [PMID] [PMCID]
6.Mannem S, Chava VK. The effect of stress on periodontitis: A clinicobiochemical study. J Indian Soc Periodontol. 2012; 16(3):365. [DOI:10.4103/0972-124X.100912] [PMID] [PMCID]
7.Sundararajan S MS, Rao SR. Relationship between depression and chronic periodontitis. J Indian Soc Periodontol. 2015; 19(3):294-6. [DOI:10.4103/0972-124X.153479] [PMID] [PMCID]
8.Caton JG, Armitage G, Berglundh T, Chapple IL, Jepsen S, Kornman KS, et al. A new classification scheme for periodontal and peri‐implant diseases and conditions-Introduction and key changes from the 1999 classification. J Periodontol. 2018; 89:S1-8. [DOI:10.1002/JPER.18-0157] [PMID]
9.AlJehani YA. Risk factors of periodontal disease: Review of the literature. Int J Dent. 2014; 2014. [DOI:10.1155/2014/182513] [PMID] [PMCID]
10.Coventry J, Griffiths G, Scully C, Tonetti M. Periodontal disease. Bmj. 2000; 321(7252):36-9. [DOI:10.1136/bmj.321.7252.36] [PMID] [PMCID]
12.Thomson WM, Sheiham A, Spencer AJ. Sociobehavioral aspects of periodontal disease. Periodontology. 2000. 2012; 60(1):54-63. [DOI:10.1111/j.1600-0757.2011.00405.x] [PMID]
13.Grossi SG, Zambon JJ, Ho AW, Koch G, Dunford RG, Machtei EE, et al. Assessment of risk for periodontal disease. I. Risk indicators for attachment loss. J Periodontol. 1994; 65(3):260-7. [DOI:10.1902/jop.1994.65.3.260] [PMID]
14.Chapple IL, Mealey BL, Van Dyke TE, Bartold PM, Dommisch H, Eickholz P, et al. Periodontal health and gingival diseases and conditions on an intact and a reduced periodontium: Consensus report of workgroup 1 of the 2017 World Workshop on the Classification of Periodontal and Peri‐Implant Diseases and Conditions. J Periodontol. 2018; 89:S74-84. [DOI:10.1002/JPER.17-0719] [PMID]
15.Holmstrup P, Plemons J, Meyle J. Non-plaque‐induced gingival diseases. J Clin Periodontol. 2018; 45:S28-43. [DOI:10.1111/jcpe.12938] [PMID]
16.Armitage GC, Cullinan MP. Comparison of the clinical features of chronic and aggressive periodontitis. Periodontology 2000. 2010; 53(1):12-27. [DOI:10.1111/j.1600-0757.2010.00353.x] [PMID]
17.Darveau RP. Periodontitis: A polymicrobial disruption of host homeostasis. Nat Rev Microbiol. 2010; 8(7):481. [DOI:10.1038/nrmicro2337] [PMID]
18.Gordis Leon. Epidemiology, 5th ed. Philadelphia: Elsevier; 2014.
19.Al-Sinaidi AA. Periodontal health and oral hygiene practice of elderly Saudis living at Riyadh Nursing Home. King Saud Univ J Dent Sci. 2012; 3(1):1-5. [DOI:10.1016/j.ksujds.2011.10.005]
20.Dinsdale CR, Rawlinson A, Walsh TF. Subgingival temperature in smokers and non‐smokers with periodontal disease. J Clin Periodontol. 1997; 24(10):761-6. [DOI:10.1111/j.1600-051X.1997.tb00194.x] [PMID]
21.Hanioka T, Tanaka M, Ojima M, Takaya K, Matsumori Y, Shizukuishi S. Oxygen sufficiency in the gingiva of smokers and non‐smokers with periodontal disease. J Periodontol. 2000; 71(12):1846-51. [DOI:10.1902/jop.2000.71.12.1846] [PMID]
22.Ketabi M, S. Hirsch R. The effects of local anesthetic containing adrenaline on gingival blood flow in smokers and non smokers. J Clin Periodontol. 1997; 24(12):888-92. [DOI:10.1111/j.1600-051X.1997.tb01207.x] [PMID]
23.Trikilis N, Rawlinson A, Walsh TF. Periodontal probing depth and subgingival temperature in smokers and non‐smokers. J Clin Periodontol. 1999; 26(1):38-43. [DOI:10.1034/j.1600-051X.1999.260107.x] [PMID]
24.Eichel B, Shahrik HA. Tobacco smoke toxicity: loss of human oral leukocyte function and fluid-cell metabolism. Science. 1969; 166(3911):1424-8. [DOI:10.1126/science.166.3911.1424] [PMID]
25.Kenney E, Kraal J, Saxe S, Jones J. The effect of cigarette smoke on human oral polymorphonuclear leukocytes. J Periodontal Res. 1977; 12(4):227-34. [DOI:10.1111/j.1600-0765.1977.tb00126.x] [PMID]
26.Kim YH, Lee JH. The relationship between oral health behavior, smoking, and periodontal diseases in Koreat middle-aged mee: based on data from the Korea National Health and Nutrition Examination Survey. 2013-2015. J Korean Acad Oral Health. 2017; 41(1):36-42. [DOI:10.11149/jkaoh.2017.41.1.36]
27.Tonetti MS, Jepsen S, Jin L, Otomo‐Corgel J. Impact of the global burden of periodontal diseases on health, nutrition and wellbeing of mankind: A call for global action. J Clin Periodontol. 2017; 44(5):456-62. [DOI:10.1111/jcpe.12732] [PMID]
28.Karasneh JA, Al Habashneh RA, Marzouka NAS, Thornhill MH. Effect of cigarette smoking on subgingival bacteria in healthy subjects and patients with chronic periodontitis. BMC Oral Health. 2017; 17(1):64. [DOI:10.1186/s12903-017-0359-4] [PMID] [PMCID]
29.ALHarthi SS, Natto ZS, Midle JB, Gyurko R, O’Neill R, Steffensen B. Association between time since quitting smoking and periodontitis in former smokers in the National Health and Nutrition Examination Surveys (NHANES) 2009 to 2012. J Periodontol. 2019; 90(1):16-25. [DOI:10.1002/JPER.18-0183] [PMID]
30.Kinane D, Attström R, B EWiPg. Advances in the pathogenesis of periodontitiss: Group B consensus report of the fifth European workshop in periodontology. J Clin Periodontol. 2005; 32:130-1. [DOI:10.1111/j.1600-051X.2005.00823.x] [PMID]
31.Wang J, Lv J, Wang W, Jiang X. Alcohol consumption and risk of periodontitis: A meta‐analysis. J Clin Periodontol. 2016; 43(7):572-83. [DOI:10.1111/jcpe.12556] [PMID]
32.Gay IC, Tran DT, Paquette DW. Alcohol intake and periodontitis in adults aged≥ 30 years: NHANES 2009-2012. J Periodontol. 2018; 89(6):625-34. [DOI:10.1002/JPER.17-0276] [PMID]
33.Lages EJ, Costa FO, Cortelli SC, Cortelli JR, Cota LO, Cyrino RM, et al. Alcohol consumption and periodontitis: Quantification of periodontal pathogens and cytokines. J Periodontol. 2015; 86(9):1058-68. [DOI:10.1902/jop.2015.150087] [PMID]
34.Kongstad J, Hvidtfeldt UA, Grønbæk M, Jontell M, Stoltze K, Holmstrup P. Amount and type of alcohol and periodontitis in the Copenhagen City heart study. J Clin Periodontol. 2008; 35(12):1032-9. [DOI:10.1111/j.1600-051X.2008.01325.x] [PMID]
35.Hach M, Holm‐Pedersen P, Adegboye A, Avlund K. The effect of alcohol consumption on periodontitis in older Danes. Int J Dent Hyg. 2015; 13(4):261-7. [DOI:10.1111/idh.12121] [PMID]
36.Suwama K, Yoshihara A, Watanabe R, Stegaroiu R, Shibata S, Miyazaki H. Relationship between alcohol consumption and periodontal tissue condition in community‐dwelling elderly Japanese. Gerodontology. 2018; 35(3):170-6. [DOI:10.1111/ger.12335] [PMID]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |